Call Us Today For FREE Consultation
“Do something today your future self will thank you for”
Cervical Myelopthy symptomps causes and treatment
Do you and/ or your loved one have neck pain? Stiffness or loss of function of neck is bothering you? We have a possible cause of your pain. Read on and get educated. Source: Barrow Neurological Institute.
Symptomps of Cervical myelopathy
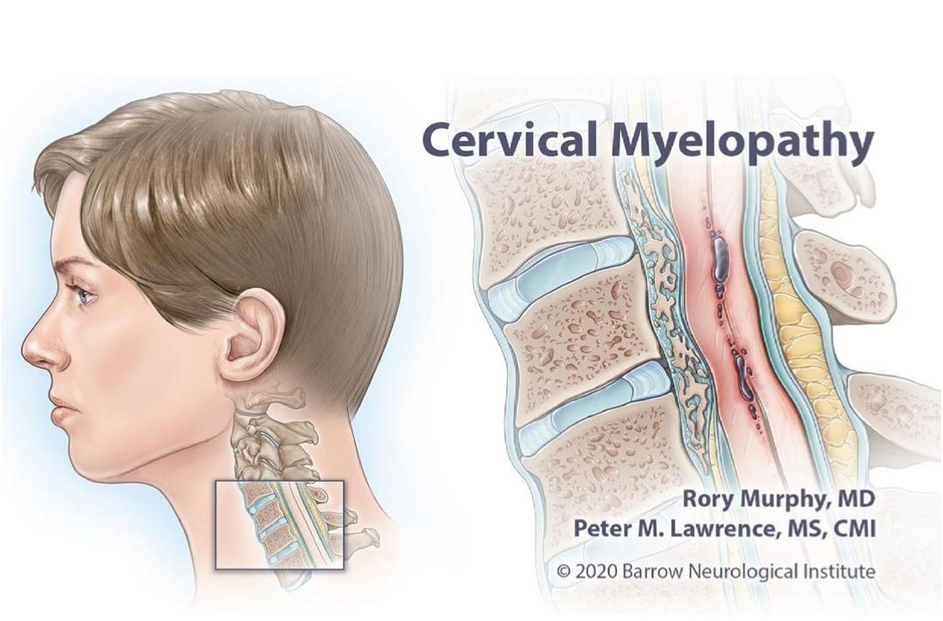
- Cervical myelopathy is a severe neurological condition. It is a moderate/severecompression of the spinal cord at the (cervical) neck level of the spinal column resulting in many motor problems.
- Cervical Myelopathy symptoms include muscle spasticity (sustained muscle contractions), hyperreflexia (muscles are more reactive of stimulus), pathologic reflexes like Babinski’s sign, digit/hand grip problems(clumsiness) and walking pattern problems (gait disturbance). Classic signs of the Cervical Myelopathy has an gradual onset that progresses in a step by step manner with functional (motor as well as sensory) decline.
- Look, without early detection and treatment, the patients may land up with significant paralysis and gross functional loss. A good therapy to delay the progression is physiotherapy. Surgery may be required in advanced cases usually a decompression of the tight area and fusion as well.
- A poor recovery prediction about Cervical Myelopathy is that symptoms worsen in a period of more than eighteen months of development. The stiffness and decreased neck (cervical spine) range of motion is evident in this stage.
- The term myelopathy is a condition that takes place from the compression of the spinal cord, whereas stenosis is the term elaborating a narrowing of a normal individual’s spinal canal. Individuals who have a congenital narrow spinal canal (born with it)care more prone to myelopathy.
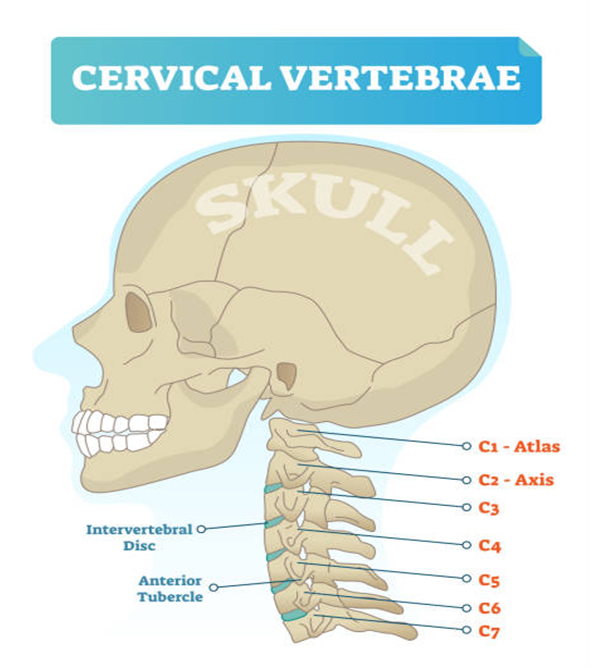
- Subsequent advancement of stenosis or a cervical disc bulge will then more likely result in myelopathy at the same cervical level. Source: spine-health.com Degenerative (which occur from old age or excess wear and tear) changes are seen at cervical vertebra level – C5 and C6 or C6 and C7, due to the more motion at cervical level.
- Additional contribution to canal narrowing are the infolding of a structure called ligamentumflavum present over the spine, an injury called spondylolisthesis (a fracture of a tiny bony structure called pars interarticularis) , needle like projections called osteophytes, and a condition called facet hypertrophy
Some common symptomps of cervical Myelopathy
- Common symptoms of Cervical Myelopathy: Distal limb (forearm, hands, lower legs, feet) weakness Decreased range of motion in the neck (cervical spine) , especially extending the neck is limited.
- Clumsy movements of hands, evident difficulty in fine motor movements writing like key holding, writing, etc.
- Pain in shoulder as well as arm. Unsteady walking pattern or clumsy gait. Increased reflexes in the lower limbs and in the upper limbs below the level of the affected area (lesion).
- Numbness and altered sensations called as paresthesia in both hands or maybe in one hand.
- Radiculopathy signs like pain running down in limbs with tingling.
- Myelopathy is likely to develop in approximately hundred percent of patients with more than sixty percent spinal canal stenosis (has less than 6 mm disc cord space).
- Progressing age is the most powerful predictor of recovery from Cervical Myelopathy and it’s perioperative morbidity as well as the neurologic recovery.
- The younger you are better are the chances of recovery. The older you get it’s difficult to recover from the spinal canal stenosis resulting in myelopathy.
Cervical Spondylotic Myelopathy:
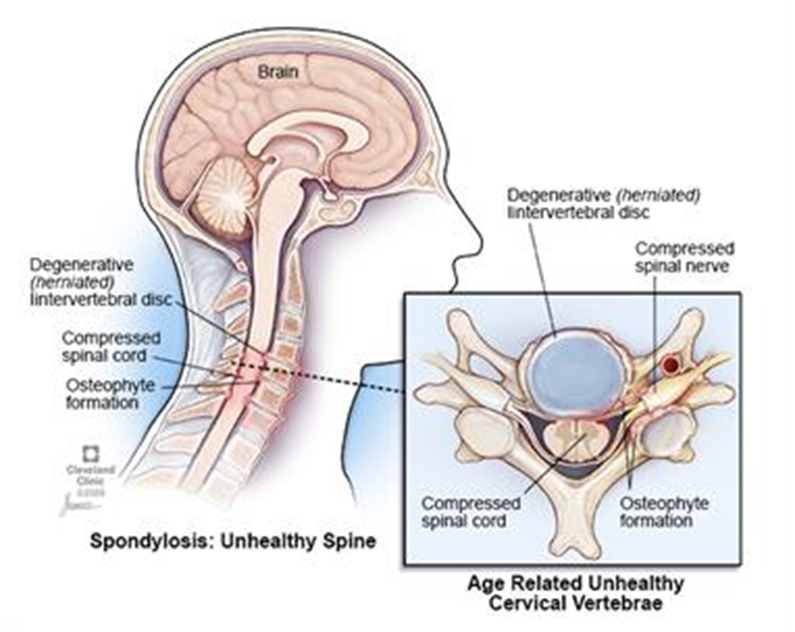
- One of the most common type of cervical myelopathy is a condition called cervical spondylotic myelopathy.
- This term “spondylosis” appertains to be one of the probable causes of myelopathy — a slow degeneration of the spine that takes place as you age. Hence, cervical spondylotic myelopathy is more frequently seen in people 50 and older.
- The gradual degeneration of the spine often results in cervical spinal stenosis, which is the narrowing of the spinal canal in the neck. Some people are born with a comparatively narrow spinal canal (congenital spinal stenosis) and they may also experience myelopathy sooner than other people if further narrowing occurs.
- Some people withbulged or herniated discs and bone spurs in the cervical vertebra are other forms of spinal degeneration that can put pressure on the spinal cord and cause myelopathy.
Other Causes of Cervical Myelopathy
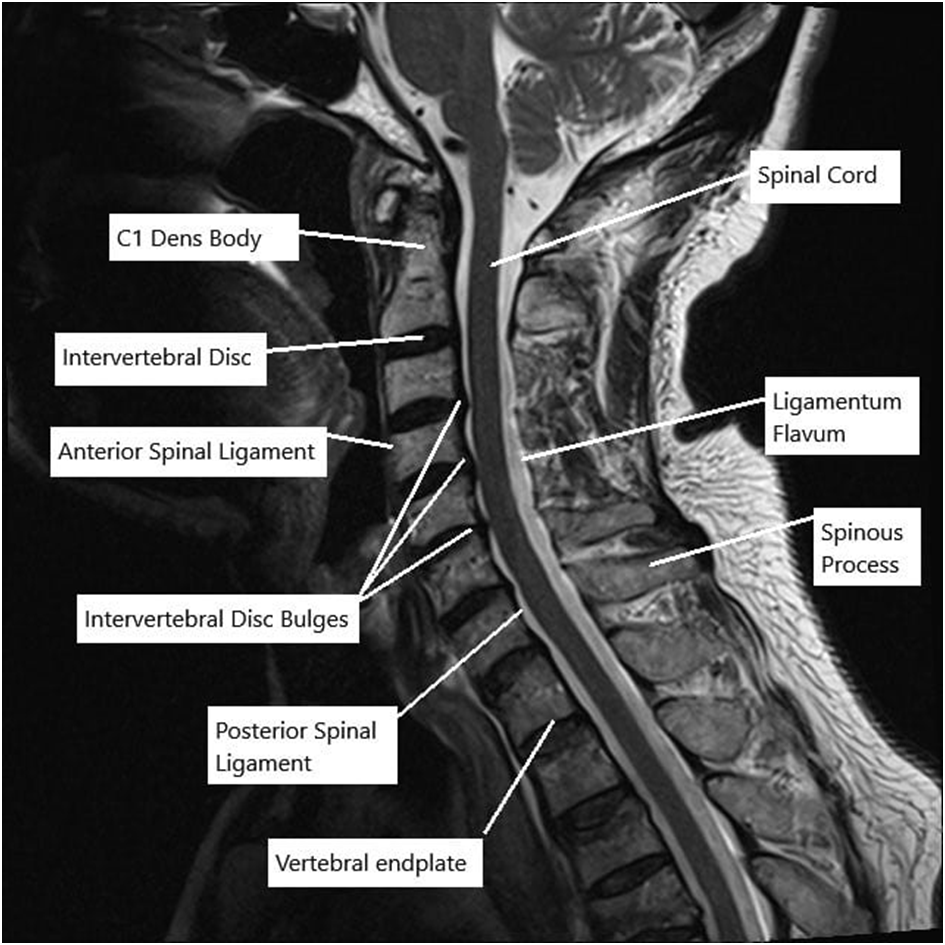
- Apart from the gradual wear and tear of the spinal vertebrae, cervical myelopathy can also be a result of ossification (hardening) of the ligaments surrounding the spinal cord, most affected ligaments are posterior longitudinal ligament and ligamentumflavu.
- The ossification of posterior longitudinal ligament (OPLL) is frequent.
- This means that the soft tissue that connects with the bones of the spinal column becomes less flexible and slowly turns into bone (ossification).
- As the age progresses the ligament thickens, it starts taking up more space and presses upon on the spinal cord, which leads to myelopathy.
- The cervical area of the spine is the most common location for Posterior Longitudinal Ligament ossification.
How is Cervical Myelopathy Diagnosed and treated?
- Xray: by visualizing the spine in different angles.
- MRI: this procedure is best to express the amount of spinal canal compression. It is considered to be the most appropriate measure for the diagnosis of compression myelopathy of a spinal cord.
- Physiotherapy Treatment: Physiotherapists can help you with all kinds of spinal problems affecting mobility and improving your quality of life.
The primary goals of physiotherapy treatment are: Overall pain relief to improve function of the affected area example: hand function to prevent the decline of neurological condition to reverse or improve the current neurological symptoms Cervical myelopathy can be treated symptomatically.

Possible therapies include:
- Cervical traction (physical as well as exercise based) and movement with manipulation of the thoracic spine: This is useful in reducing the pain and level of disability in individuals with mild cervical myelopathy.
- Other signs and symptoms, such as weakness, headache, dizziness, and loss of sensation, can also be positively affected. Cervical traction can be combined with other treatments like electrotherapy and exercises.
- A study done by Joghataei et al. reported a significant rise in grip strength after 10 weeks of this combined treatment.
Manual therapy techniques:

- Manual therapy techniques are used for the improvement in neck pain with a technique called natural apophyseal glides and sustained natural apophyseal glides for better neck turns and neck extending (cervical extension and rotation). Manipulation and mobilisations are effective when they are combined with exercise therapy.

Some techniques are performed by your Physiotherapist and some will be taught by the Physiotherapist to you.
Caution: Self mobilisation is taught and done under an experienced Physiotherapist. Be careful and vary about anything you see which is not taught to you. Exercises: All kinds of mobility exercises benefit the stiffness and decreased range of motion of neck.
- Exercises including stretching, resistance band exercises, PNF exercises are prescribed and taught by our experts to minimize your pain and increase mobility. Many new techniques and equipments are used to increase the neck range of motion and to to maintain the strength and flexibility of muscles.

Cervical stabilization exercises: When there is evident instability of the vertebral bodies of a degenerative type.
- Biofeedback:

- An equipment called the pressure biofeedback unit is used to stabilize and yet activate the cervical muscles. Your physiotherapist will instruct you how to stabilize the vertebral instability of the cervical spine.
- Balance training If you already have balance issues your physiotherapist will teach you balance retraining exercises to prevent fall.
- Balance training is helpful for proprioception (awareness of body position), it can be done with and without equipment. There are exercise equipment used by the physiotherapists to improve balance such as balance pads.
- Core stability exercises: Core stability exercise will be taught by one of our experts to tighten the muscles of the abdomen and back to keep the spine straight.
- These exercises help in maintaining optimum posture and prevent further compression of the spinal cord.
How progressive care treat Cervical Myelopathy?
- In surgical cases, the physiotherapist has an important role, before and after the surgery. In the pre-operative phase, the physiotherapist needs to be thoroughly aware with the patient’s history, occupation and about their activities they perform in daily living. What are the activities that the patient is aiming to return to?
- The physiotherapist will inform you about the physiotherapy treatment program and the possible outcomes after the surgery. Exercises to improve mobility and proprioception will be taught by the physiotherapist. The patient starts with stabilisation exercises after the post surgery healing period and then Physiotherapist will guide you through more active mobilization exercises.
- During the day the patient is encouraged to perform their usual ADLs. The Physiotherapist will alter the intensity of the exercises depending upon the performance and you will be progressed towards activities that include standing and walking. Physiotherapist will help you to adapt all activities in the home environment with active exercises.
- You will be taught every modified way to perform the normal activities of daily living. You will be monitored and the Physiotherapist will increase the intensity of the exercises as needed.
Reference:
- A Clinical Practice Guideline for the Management of Degenerative Cervical Myelopathy: Introduction, Rationale, and Scope Michael G.
- Fehlings, MD, PhD, FRCSC, FACS, Lindsay A. Tetreault, PhD, […], and Jeffrey C.Wang MD Leonardi M, Boos N. Degenerative disorders of the cervical spine.
- Spinal Disorders 2008 (pp. 429-479). Springer, Berlin, Heidelberg. Kadanka Z, Bednarík J, Novotný O, Urbánek I, Dušek L. Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. European Spine Journal.
- 2011 Sep;20(9):1533-8 Joghataei MT, Arab AM, Khaksar H. The effect of cervical traction combined with conventional therapy on grip strength on patients with cervical radiculopathy.
- Clinical rehabilitation. 2004 Dec;18(8):879-87. Ogawa Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, Toyama Y. Postoperative factors affecting neurological recovery after surgery for cervical spondylotic myelopathy.
- Journal of Neurosurgery: Spine. 2006 Dec 1;5(6):483-7. Management of spinal cord injury by Lisa Harvey. Chapter 2, 7,8 and Chapter 12.

Progressive Care Physiotherapy
Progressive Care Physiotherapy Management is the best service in the physiotherapy industry. It is known for providing the best service and cutting-edge technology to help speed up recovery, while also being able to offer various treatment options that are tailored to your specific needs.
For More details call us on 9618906780
